Johnson & Johnson’s recent vaccine announcement has sparked great hope in the United States, with virus experts calling it a potential “game changer.” In a Jan. 29 press release, the company announced that their single-shot COVID-19 vaccine had demonstrated broad success at preventing moderate to severe infection from the SARS-CoV-2 virus. As the U.S.’s vaccine rollout continues to struggle through complaints of statewide shortages, the prospect of a third vaccine circulating in the country is certainly cause for excitement.
By all metrics, J&J’s vaccine is a success at 72% efficacy. It far surpasses the efficacy of a normal flu vaccine, which can range from 40% to 60% effective in any given year. No American should feel that the J&J vaccine isn’t effective enough to be worth getting.
However, its rate still lags significantly behind its counterparts. The other two vaccines authorized for use in the U.S., developed by Moderna and Pfizer-BioNTech, proved 94% and 95% effective, respectively. That means that as J&J’s vaccine approaches the market, healthcare officials will face the dilemma of fairly allocating the less effective vaccine. Why would someone at high risk for severe COVID-19 complications want to take a slightly less protective product if a better option is readily available?
The ethical method of allocation is prioritizing the J&J vaccine’s use in younger and lower-risk patients and keeping the more effective vaccines for use elsewhere.
When the Pfizer and Moderna vaccines were first authorized for use in the U.S., the Center for Disease Control laid out a vaccine prioritization recommendation designed to make sure doses were ethically allocated to our nation’s most vulnerable populations. The plan’s phases 1a through 1c suggest healthcare workers and long-term care facility residents should get the vaccine first; then frontline essential workers and people 75 and older; then other essential workers, people over age 65, and people with high-risk medical conditions.
Only after those priority groups are vaccinated will the rest of the population have access.
But since Johnson & Johnson’s vaccine is only 72% effective at preventing moderate to severe Covid-19, it might actually be more advantageous to use it among populations that are already less susceptible to extreme illness from the virus.
People in the age groups between 18 and 49 account for less than 5% of deaths in the United States. However, those same age groups are responsible for more than 50% of cases in the U.S., with 18 to 29-year-olds accounting for more than 20% on their own. Though they are often spared from deadly infection themselves, these groups spread the virus to other higher-risk populations. Vaccinating them and stopping their spreading of the virus is another essential step in establishing herd immunity in the U.S.
That’s not to say young people who break CDC protective guidelines should be rewarded by getting the vaccine early. Still, even in Phase 1, there were many young and healthy people vaccinated under early priority. Phases 1b and 1c included roughly 87 million essential workers, only a third of whom are over the age of 50. That leaves over 50 million early-priority individuals in the age groups that suffer the fewest casualties from COVID-19.
Most of those people could receive the Johnson & Johnson vaccine without assuming much additional risk, leaving more of the Moderna and Pfizer vaccines for use elsewhere.
At the moment, the majority of states are struggling to get just their at-risk populations vaccinated. But as we progress through 2021, some states have caught up, saying they don’t have enough vaccines to maintain maximum distribution capabilities or to reach President Biden’s goal of 100 million vaccines in his first 100 days. Most are hopeful that the Johnson & Johnson vaccine will supply additional doses to keep up with demand.
Unfortunately, J&J’s vaccine might not hit the shelves until mid-March. While it has reportedly passed most safety benchmarks, a delay is anticipated as the FDA considers it for emergency authorization. That means that the vaccine distribution could be nearing availability to the general public before J&J’s product can even reach the market.
Regardless, Johnson & Johnson’s 100 million doses anticipated by the end of June should go a long way toward protecting the public from the ever-deadlier pandemic. And while we must reckon with the disparity between each vaccine’s efficacy, prioritizing the Johnson & Johnson vaccine for less vulnerable populations each step of the way will ensure immunization can be accomplished in the most ethical and equitable way.
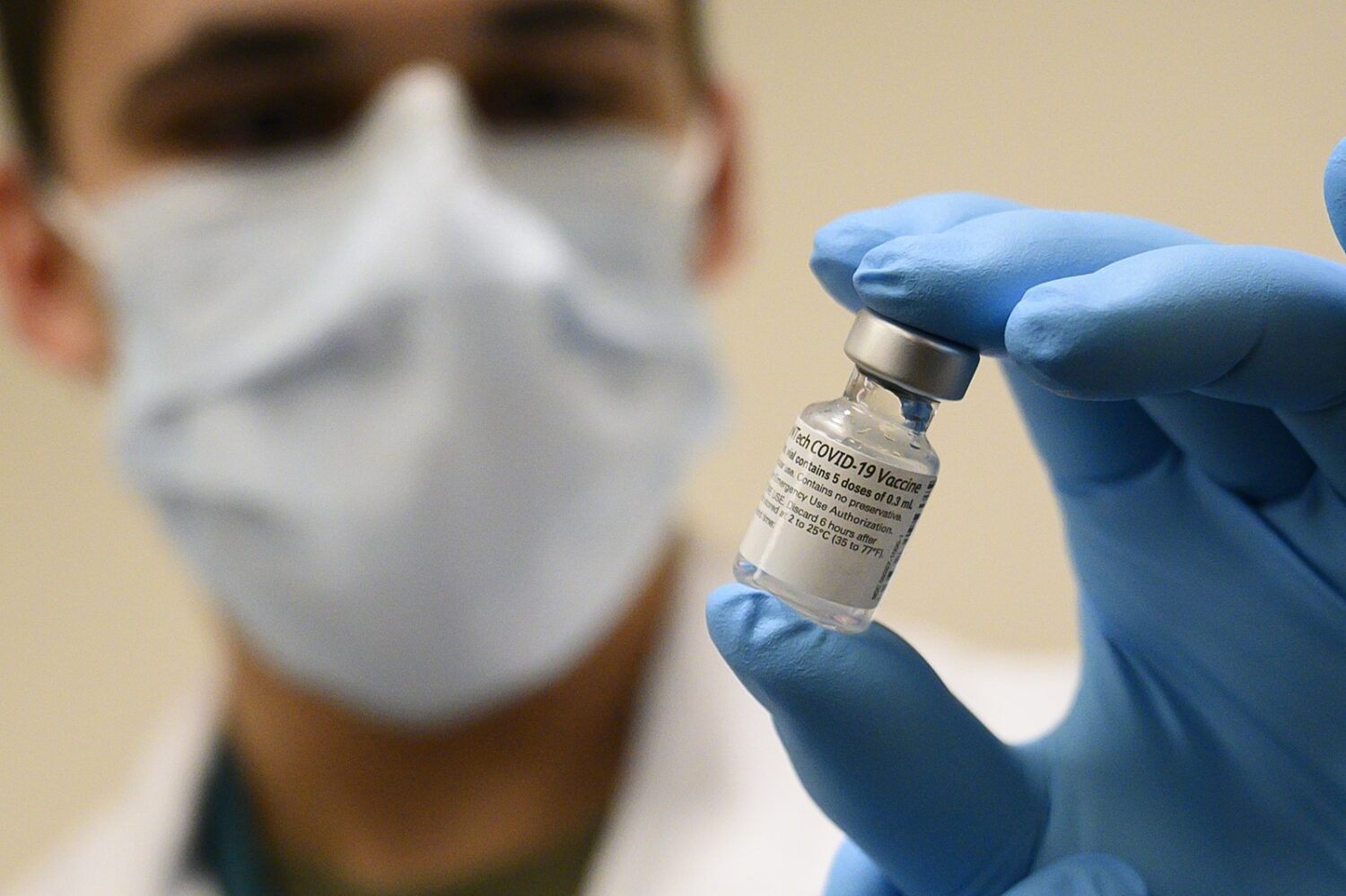
Image Credit: The photo from the U.S. Secretary of Defense is licensed under CC BY 2.0.